Correlation of responsiveness to pain intensity and functional status measurements after lumbar epidural steroid injection in patients with lower back pain
Article information
Abstract
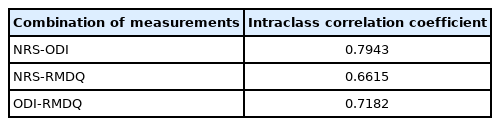
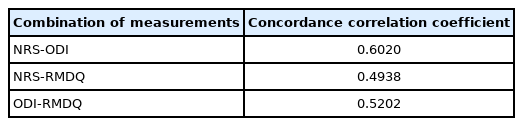
This study aimed to examine the changes in the Numerical Rating Scale (NRS), Oswestry Disability Index (ODI), and Roland Morris Disability Questionnaire (RMDQ) scores before and after epidural steroid injection (ESI) in patients with lower back pain, and the correlation between the three scales in patients with reduced scores on these scales. Patients completed the NRS, ODI, and RMDQ before and after receiving ESI. A paired t-test was performed to compare the mean scores obtained before and after ESI. The correlations between the scores were estimated by calculating the difference between the baseline and follow-up scores. Of the 49 patients, 37 completed both questionnaire assessments. Among them, 26 patients (70%) presented a post-ESI decrease in scores obtained on all three scales. The NRS score decreased from 6.81±1.91 points at baseline to 3.66±2.22 points at follow-up (p<0.0001); similarly, the ODI score decreased from 41.65±14.76 to 30.38±16.16 points (p=0.0025); and the RMDQ score decreased from 11.11±5.68 to 7.64±5.74 points (p=0.011). Of the 37 patients who completed the two questionnaires, 26 had reduced NRS, ODI, and RMDQ scores. The intraclass correlation coefficients between the NRS and ODI, NRS and RMDQ, and ODI and RMDQ scores were 0.7943, 0.6615, and 0.7182, respectively. The concordance correlation coefficients between the NRS and ODI, NRS and RMDQ, and ODI and RMDQ scores were 0.6020, 0.4938, and 0.5202, respectively. Among the measurements, the correlation between the NRS and ODI scores was the highest, and a moderate correlation was found between the scores obtained using the other instruments.
INTRODUCTION
Lower back pain (LBP) affects 70-85% of people at least once in their lifetime, with an annual prevalence in the range of 15-45% [1]. Epidural steroid injection (ESI) under fluoroscopic guidance is reportedly effective in managing LBP [2]. LBP is typically measured using instruments such as the Visual Analog Scale (VAS) and Numerical Rating Scale (NRS), which may help assess the efficacy of treatment by providing an objective score for the subjective experience of pain. However, both VAS and NRS disregard the emotional and functional aspects of LBP and are considered inadequate for identifying individual differences in chronic LBP and changes in symptoms [3]. In response to these limitations, specialized questionnaires, such as the Oswestry Disability Index (ODI), Roland Morris Disability Questionnaire (RMDQ), and Quebec Back Pain Disability Scale, have been developed to assess the functional status of patients with LBP, particularly those undergoing surgery or rehabilitation [4]. The recovery of patients with LBP depends on their appraisal of the impact their symptoms have on their daily lives, including their ability to fulfill social roles, rather than the crude presence or absence of pain [5]. This finding suggests that LBP should be assessed using multidimensional tools. The association between the VAS and NRS scores and the ODI or RMDQ scores, and the effectiveness of ESI in LBP treatment remains controversial. This study aimed to examine the changes in the NRS, ODI, and RMDQ scores before and after ESI in patients with LBP and the correlation between the three scales in patients with reduced scores on the three scales.
METHODS
This prospective study was conducted between March 2016 and February 2017 and was approved by the Review Board of Jeju University Hospital (Approval no. 2017-05-005-002). The age range of the study participants was 20-80 years; all patients complained of LBP and presented to our outpatient pain clinic. In total, 49 patients were enrolled in this study. The aims of the study were explained, and informed consent was obtained from all patients. Patients with difficulties in understanding the contents of the consent form due to mental or physical disability and those who required a representative to provide consent were excluded from this study. Patient characteristics of interest were sex, age, diagnosis, and the type of ESI received. The patients completed the NRS, ODI, and RMDQ assessments before and 2 or 4 weeks after receiving ESI.
The NRS is an 11-point scale, with pain scores ranging from 0 (“no pain”) to 10 (“most severe imaginable”). The degree of disability was measured using the Korean versions of the ODI and RMDQ. The ODI assesses pain (one item) and activities of daily living (personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling; nine items). The maximum ODI score is 50 points, and disability is scored from 0 (“no disability”) to 5 (“severe disability”). The RMDQ measures the degree of disability in everyday life using 24 items that assess pain, sleep, appetite, and emotional function, yielding a total score of 24 points [4].
1. Statistical analysis
A paired t-test was performed to compare the mean and standard deviation of the NRS, ODI, and RMDQ scores before and after ESI. Correlations between the NRS, ODI, and RMDQ scores were estimated using the intraclass correlation coefficients (ICCs) and concordance correlation coefficients (CCCs), obtained by calculating the difference between the baseline and follow-up scores and converting this value to a percentage score as follows: ([pre-value - post-value/pre-value]×100). The ICC was calculated to determine the level of intermeasure agreement for improvement after ESI; it was categorized as excellent (0.75- 1.0), good (0.6-0.75), fair (0.4-0.6), and poor (<0.4). The CCC was calculated to determine the level of agreement for improvement after ESI between the measurements and was categorized as excellent (0.81-1.00), good (0.61-0.80), moderate (0.41-0.60), fair (0.21-0.40), and poor (<0.20) [6]. Statistical calculations were performed using the R software version 3.6.2 (R Project for Statistical Computing, Vienna, Austria), except for ICC and CCC calculations, which were performed using Medcalc (Medcalc Software; Mariakerke, Belgium). Statistical significance was set at P<0.05.
RESULTS
Of the 49 patients, 37 completed two questionnaires (Table 1). The NRS scores decreased from 6.81±1.91 points at baseline to 3.66±2.22 points at follow-up (P<0.0001) (Fig. 1A). The ODI and RMDQ scores decreased from 41.65±14.76 to 30.38±16.16 points (P=0.0025), and from 11.11±5.68 to 7.64±5.74 points (P=0.0111), respectively (Fig. 1B, C). After conversion to percentage scores, the values were 45.68±27.96%, 23.01±45.14%, and 30.62±51.09%, respectively. The NRS and RMDQ scores decreased, and the ODI score increased after ESI in five patients. The NRS and ODI scores decreased, and the RMDQ score increased in two patients. The NRS score decreased; however, the ODI and RMDQ scores increased in three patients. The ODI and RMDQ scores decreased, and the NRS score increased in one patient. In addition, 26 patients (70%) reported a decrease in scores on all three scales after receiving the ESI (Fig. 2).
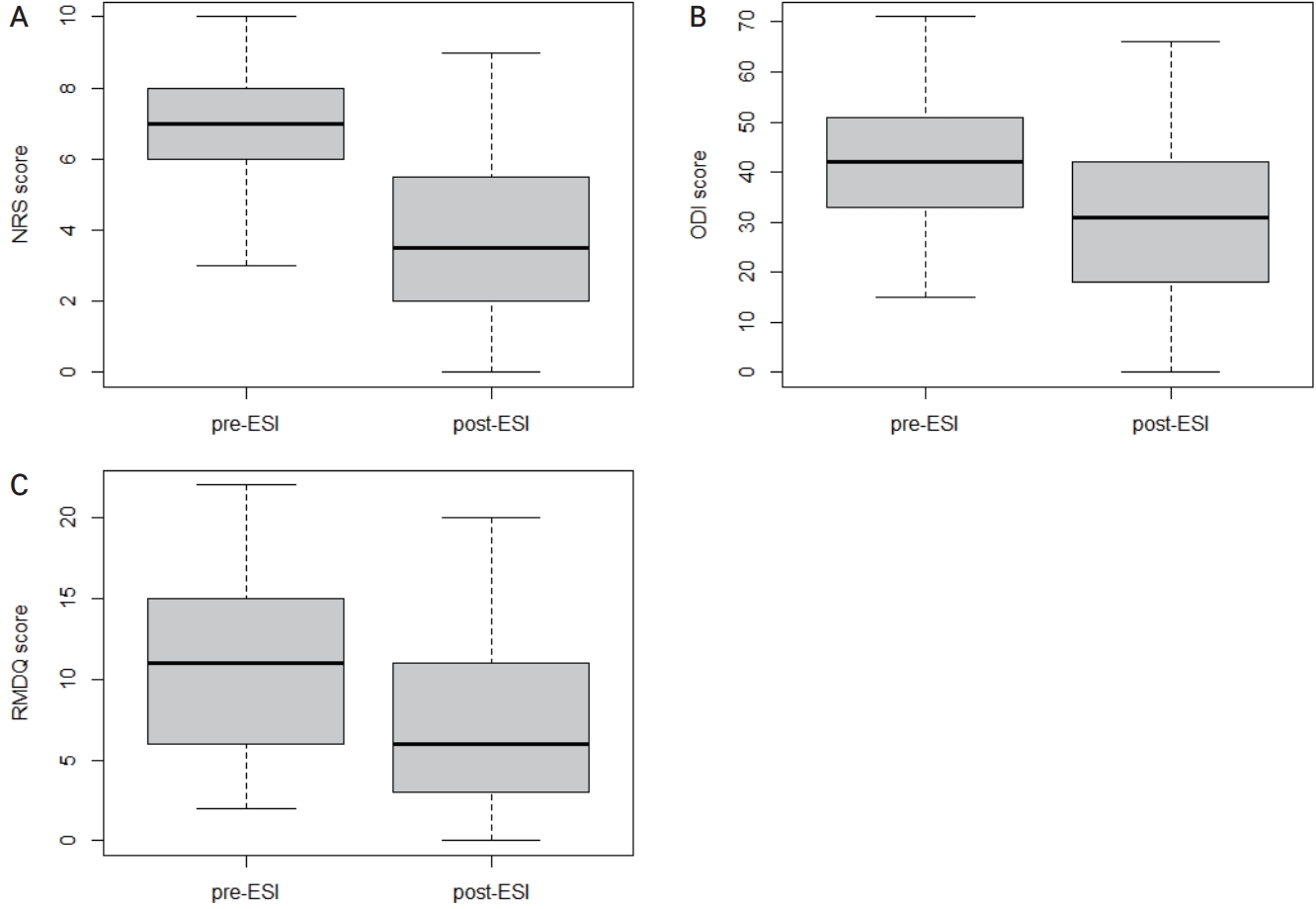
(A) NRS, (B) ODI, and (C) RMDQ. Pre-ESI and 2 or 4 weeks post-ESI. NRS: Numerical Rating Scale, ODI: Oswestry Disability Index, RMDQ: Roland Morris Disability Questionnaire, ESI: epidural steroid injection.
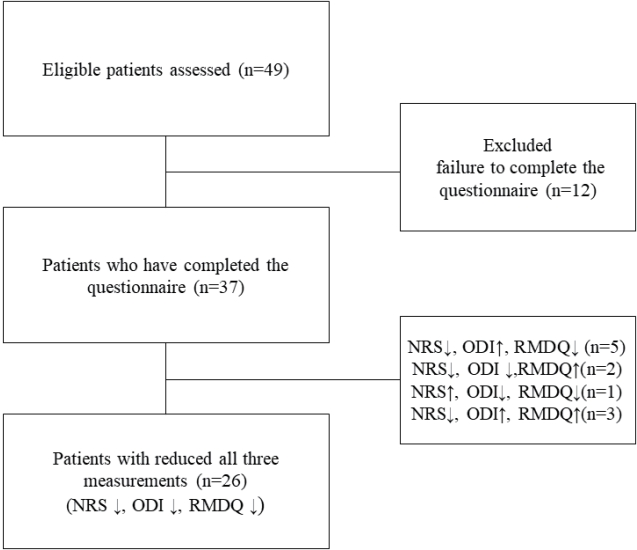
Patient enrollment algorithm. NRS: Numerical Rating Scale, ODI: Oswestry Disability Index, RMDQ: Roland Morris Disability Questionnaire.
The ICC for the NRS and ODI scores was 0.7943, which was the highest in the present study. The CCC between the NRS and ODI scores was 0.6020 (95% confidence interval, 0.31-0.79), with precision and accuracy estimates of 0.66 and 0.91, respectively (Tables 2, 3).
DISCUSSION
The NRS is a one-dimensional tool used to measure the subjective intensity of pain; it is challenging to measure the multidimensional characteristics of pain [7]. The ODI and RMDQ measure LBP-related disability and are commonly used questionnaires in studies on patients with LBP [8]. Therefore, the ODI and RMDQ were used in this study for the functional evaluation of LBP before and after ESI. Hush et al. [5] reported that the determinants of recovery from LBP were symptom control, improvement of function, and quality of life. As no single measurement can adequately determine the progression of emotional, functional, and symptomatic improvement or regression in patients with LBP, this study evaluated the effects of ESI using different outcome measures.
However, the correlation between NRS and ODI in evaluating patients with LBP who undergo nerve block is controversial because the results vary in the literature.9,10) Additionally, the RMDQ is considered a comprehensively validated measure in patients with LBP, and there is no literature that uses the RMDQ to evaluate LBP before and after ESI and analyze the correlation with NRS. Therefore, in this study, the correlation between the two measurements of the ODI, RMDQ, and NRS was analyzed.
In this study, 26 patients (70%) presented with a decrease in scores on all three scales after the ESI. Among these patients, the correlation between the NRS and ODI scores was the highest, whereas a moderate correlation was found between the scores obtained by the other scales. Barre et al. [11] reported that patients who underwent fluoroscopically guided caudal ESI showed an improved VAS and RMDQ scores for up to 2.5 years after receiving injections. Meanwhile, Botwin et al. [12] reported that patients who underwent fluoroscopically guided lumbar transforaminal ESI had improved VAS and Roland 5-point pain scale scores, standing/walking tolerance, and satisfaction levels for up to 12 months after injections. In this study, these three measurements decreased significantly. However, the minimal clinically important difference in LBP score values varies among studies. Despite differences in disease progression and affected areas, a 2-3 point reduction in the NRS has been suggested as meaningful [13]. Other estimates are in the range of 4-16 (ODI) and 3-5 (RMDQ) points [14]. In the present study, the NRS, ODI, and RMDQ scores decreased by 3, 16, and 5 points, respectively, relative to the baseline; these differences were statistically significant.
However, previous studies on the correlations between different outcome measurements have reported discrepant findings. For example, Tomkins-Lane et al. [15] reported that 17 patients treated with fluoroscopically guided ESI for symptomatic spinal stenosis had improved VAS scores; however, their ODI scores increased. In addition, Seo et al. [9] reported that 164 patients with neck or back pain who received spinal injections experienced changes in their symptoms, expressed in the NRS and ODI scores, neck disability index, residual symptom percentage, and global perceived effect assessment. This study showed good concordance between the residual symptom percentage and global perceived effect assessment and poor agreement between the NRS and ODI scores [9].
Lee et al. [7] proposed that using a pain relief scale with the NRS increased the objectivity of pain assessment and compensated for the shortcomings associated with using only the VAS or NRS scales. The Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials has endorsed the RMDQ as an outcome measure in patients with LBP [16]. In contrast, Hush et al. [17] suggested that the NRS and RMDQ were inadequate for assessing the complexity of pain in adults with persistent LBP. Meanwhile, Theodore et al. [18] evaluated pain reduction after performing a diagnostic facet block using the NRS and global perceived improvement (GPI) scale, showing no concordance between the corresponding scores. The NRS evaluates current pain intensity, while the GPI scale assesses the overall experience of pain reduction and depends on numerous factors such as current pain, pain intensity recall, and mental subtraction [18].
In the present study, the patients were asked to evaluate the intensity of pain and other functional aspects in real time. Although patients tend to overestimate their pain levels, the impact of nerve blocks such as ESI may be accurately assessed using such assessments. In this study, after ESI, the ICC between the NRS and ODI scores was excellent (0.7941), and the CCC was 0.6057, which was the highest value in the present study. The ODI is commonly used to measure disability in patients with LBP; it is considered more sensitive in patients with persistent and severe disability than the RMDQ [8,19]. The RMDQ is useful for evaluating patients with mild to moderate disabilities and measuring changes in LBP over time [17,20]. In the present study, most patients presented with severe pain and highextent disability at baseline.
The limitations of the present study include the small sample size and the short period between baseline and follow-up assessments. In addition, this study did not consider the pain type (acute vs. chronic). Treatment with nerve blocks, such as ESI, is more effective in acute pain than chronic pain. Third, the severity of the degenerative changes in the spine was not assessed. Further research is required to identify a tool suitable for pain evaluation after nerve block treatment.
In conclusion, in the present study, 26 patients (70%) presented with a decrease in scores on all three scales after ESI. Among these patients, the correlation between the NRS and ODI scores was the highest; a moderate correlation was found between the scores obtained using the other instruments.
If The NRS and ODI are measured together in patients with LBP, the shortcomings of NRS can be supplemented and LBP before and after ESI can be evaluated more effectively.