Comparison of the Korean Activity Status Index with cardiopulmonary exercise test in patients with acute myocardial infarction
Article information
Abstract
This study aimed to compare the Korean Activity Status Index (KASI) with the cardiopulmonary exercise test (CPET) among patients with acute myocardial infarction. A total of 2,268 patients (85.4% male; mean age, 59.3±10.2 years; range, 23-90 years) diagnosed with acute myocardial infarction were enrolled in the Regional Center Myocardial Infarction Registry between July 2016 and June 2019. The KASI is a tool used to measure functional capacity by asking patients about their ability to perform specific activities and then scoring their responses. In contrast, CPET is the gold standard for assessing the objective functional capacity in patients undergoing cardiac rehabilitation. Peak oxygen uptake (VO2peak) was used to analyze the correlation. Patients who completed two consecutive KASI and CPET evaluations during their first (KASI_1, VO2peak_1) and second visits (KASI_2, VO2peak_2) for cardiac rehabilitation were included in the study. The mean KASI_1 and KASI_2 scores were 43.3±14.3 and 49.8±13.9, respectively, and the mean VO2peak_1 and VO2peak_2 scores were 25.9±8.0 and 28.5±8.3, respectively. Both the KASI scores were significantly correlated with the measured VO2peak during each visit, with correlation coefficients of 0.385 (P<0.001) and 0.346 (P<0.001), respectively. Moreover, the KASI score and VO2peak had a linear relationship (VO2peak_1=0.22×KASI_1+16.5, P<0.001; VO2peak_2=0.21×KASI_2+18.2, P<0.001). This study revealed that the KASI is a valid measure for the follow-up evaluation of the functional capacity of patients. These findings suggest that VO2peak can be predicted using the KASI score in patients who do not undergo CPET.
INTRODUCTION
Cardiovascular diseases (CV Ds), especially acute myocardial infarction (AMI), are a leading cause of death worldwide [1]. In Korea, CVDs have the second highest mortality rate after cancer, with an increasing trend in recent years. Moreover, the trend of AMI incidence for the period of 2007-2016 showed a decrease until 2011 and then increased until 2016 [2]. Patients with AMI often experience a marked decline in physical function, resulting in decreased activities of daily living (ADL) and health-related quality of life (HRQoL) [3,4].
Cardiac rehabilitation (CR) is an important intervention in the secondary prevention of CVDs and aims to improve functional capacity, HRQoL, and recovery in the physical and psychological areas among patients with heart disease [5-8]. Several studies have established that exercise-based CR results in a significant reduction in the risk of reinfarction through improved cardiac and coronary vascular function, as well as mortality, when compared to CR without an exercise component [6,9,10]. Therefore, there is a need for an accurate and reliable measurement method to assess individual patient function in the actual clinical setting.
The assessment of functional status provides information on the patient’s physical ability, general condition, and prognosis [8,11]. Questionnaires and objective tools are the most commonly used measurements to assess functional activity. Cardiopulmonary exercise testing (CPET) with the measurement of peak oxygen uptake (VO2peak), currently considered the gold standard for assessing functional capacity, is a dynamic, symptom-limited, and noninvasive test for cardiovascular disease [12,13]. CPET is relatively time-consuming and expensive to perform, and cannot be performed in situations such as physical impairment (e.g., severe muscle weakness, recent orthopedic surgery, or acute pain) and cognitive decline [8].
The HRQoL assessment in CR is essential because it represents the patient’s self-assessment of the disease effects on their physical function and well-being [6,7,14]. Recently, various evaluation tools, such as the Medical Outcome Study Short Form 36 and MacNew Heart Disease Health Quality of Life Questionnaire, Duke Activity Status Index (DASI), and Korean Activity Scale/Index (KASI) have been used for HRQoL evaluation [6,7,15,16].
As one of several evaluation indicators, the KASI is the first functional performance scale assessment tool developed for Koreans and is useful in measuring an individual’s functional status and ability to perform certain activities. It is a self-report questionnaire that determines whether certain activities in daily life can be performed by patients with CVDs. Moreover, the KASI scores can be evaluated even when CPET is difficult to perform. In addition, it has been proven to be a simple and useful tool that can be used in clinical research [16].
Nevertheless, there are no studies on the correlation between the KASI score and CPET findings, especially VO 2 peak. Therefore, the main aim of this study was to evaluate the relationship between the KASI and CPET, which are two reliable tools for patients with myocardial infarction. A correlation between the KASI and CPET indicators may mean that doctors could consider prescribing an exercise using the KASI score when the patient has difficulty performing CPET.
METHODS
1. Overview of the Korean Registry of Acute Myocardial Infarction for Regional Cardio-cerebrovascular Centers (KRAMI-RCCs)
The KRAMI-RCCs was founded in 2008, with 14 participating hospitals. The main goal of the KRAMI-RCCs is to operate a daily and hourly treatment system for the timely treatment of patients with AMI and stroke and to conduct patient education and rehabilitation for secondary prevention. In July 2015, a team of diverse experts (including cardiologists, rehabilitation physicians, preventive medical physicians, government stakeholders, and web developers) began developing web-based KRAMI-RCCs. The first data from the KRAMI-RCC were registered on July 1, 2016. All users of the 14 RCCs entered the online registry data of patients with AMI from their hospital records [17].
After admission, all participants were informed of the study purpose and consented to participate in the study program. This study was approved by the Institutional Review Board (IRB) of Jeju National University Hospital (IRB No. 2020-01-007).
2. Study design
This was a retrospective observational multicenter registry study that evaluated the correlation between the KASI score and CPET findings in patients with AMI.
3. Participants
A total of 11,894 registered patients who had used the emergency room services of each participating institution and were diagnosed with A MI were en rolled in the KRAMI-RCCs from July 2016 to June 2019. Participants who received inpatient treatment and were referred to the Department of Rehabilitation Medicine for all assessments were included in the study.
Out of a total of 11,231 screened patients, 2,916 were subjected to the primary evaluation: KASI_1 and VO2peak_1. Patients who did not complete all evaluations owing to distance, time, and economic issues, as well as loss of contact, death, or readmission to the hospital because of reinfarction during the follow-up period, were excluded from the study. A total of 2,268 patients were finally enrolled in this study (Fig. 1).
4. Outcome measurements
1) Cardiopulmonary exercise test
CPET is a widely applied assessment tool for the objective analysis of the functional ability of patients undergoing cardiac rehabilitation using electrocardiogram stress testing and ventilation gas analysis. That is, all the air inspired and expired by the patient during the examination is collected and analyzed [12,13]. In this study, VO2peak, a parameter derived from CPET, was used to analyze the correlation between the KASI score and CPET. Peak exercise cardiopulmonary responses were evaluated using symptom-limited progressive exercises. All patients were assessed in a standardized CPET, ref lecting their individual condition. The exercise test was terminated upon patient request or if gait instability or cardiovascular decompensation, determined according to the guidelines of the American College of Sports Medicine [18], was observed.
2) Korean Activity Status Index
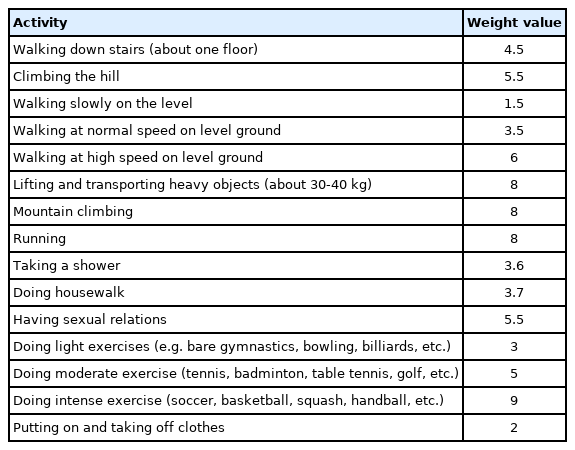
All participants completed a questionnaire that assessed 15 physical activities associated with ADLs (e.g., climbing stairs, walking on level ground, carrying heavy objects weighing approximately 30-40 kg, or sexual intercourse). Each activity was also associated with an activity-specific value. The participants were asked to identify each activity that they were able to perform. The total scores that ranged from 0 to 78.6 were weighted according to the grading guidelines (Table 1). The higher the total score, the better was the degree of functional performance. During the validation, the reliability coefficient was 0.81 [16].
All participants were assessed at 1 and 3 months after AMI diagnosis. They completed two consecutive KASI and CPET evaluations during their first (KASI_1 and VO2peak_1) and second (KASI_2 and VO2peak_2) visit. Well-trained coordinator nurses collected all data, including patient demographics, disease-related characteristics (infarction lesion, comorbidities, and smoking history), objective measures of CPET-derived VO2peak using gas exchange analysis, and KASI scores.
5. Statistical analysis
The association between the KASI score and peak oxygen uptake derived from CPET was measured using Pearson’s correlation coefficient. Based on the collected data, we calculated the predicted VO2peak derived from the equation between the KASI score and CPET. We then assessed the bias and 95% limits of agreement between the actual measured and predicted VO2peak using a Bland-Altman plot. 19,20) A scatter plot was used to assess the correlation between the measured VO2peak and the KASI-predicted VO2peak.
All statistical analyses were performed using SPSS for Windows (version 18.0; SPSS Inc., Chicago, IL, USA) and MedCalc version 19 (MedCalc Co, Ostend, Belgium). Statistical significance was set at P<0.05.
RESULTS
1. Demographic and disease-related characteristics
The demographic and disease-related characteristics of the participants are presented in Table 2. The mean age was 59.3±10.2 years and 85.4% of the participants were male. Among these patients, 1,031 (45.5%) had ST-elevation myocardial infarction and 1,237 (54.5%) had non-ST-elevation myocardial infarction. The left anterior descending artery was the most frequently involved artery (46.8%). Among these patients, those with AMI had the following comorbidities: hypertension (40.9%), diabetes mellitus (22.1%), and dyslipidemia (12.9%). A total of 1,064 participants were current smokers, and 464 participants were past smokers who had stopped smoking for at least 1 year.
2. Comparison of the KASI scores and predicted- and measured-VO2peak
Table 3 compares the KASI scores and the predicted- and measured-VO2peak values. The mean KASI_1 and KASI_2 scores were 43.3±14.3 and 49.8±13.9, respectively, whereas the mean VO2peak_1 and VO2peak_2 were 25.9±8.0 and 28.5±8.3, respectively.
3. Correlation between the KASI score and CPET findings
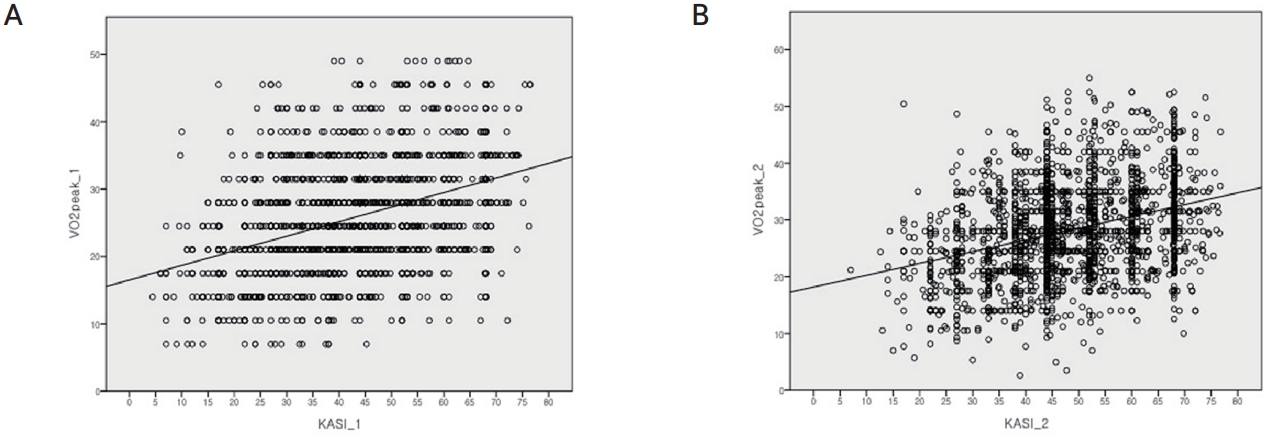
Fig. 2 shows the cor relation bet ween K ASI_1 and VO2peak_1 and between KASI_2 and VO2peak_2. Both the KASI scores were significantly correlated with the measured VO2peak during each visit, with correlation coefficients of 0.385 (P<0.001) and 0.346 (P<0.001), respectively. There was a linear relationship between the KASI score and VO2peak at each time point. Based on the linear relationship at each period, we obtained the following statistically significant equation: VO2peak_1= 0.22×K ASI_1+16.5, P<0.001; VO2peak_2=0.21×KASI_2+18.2, P<0.001.
4. The bias and 95% limits of agreement between the KASI-predicted and CPET-measured VO2peak
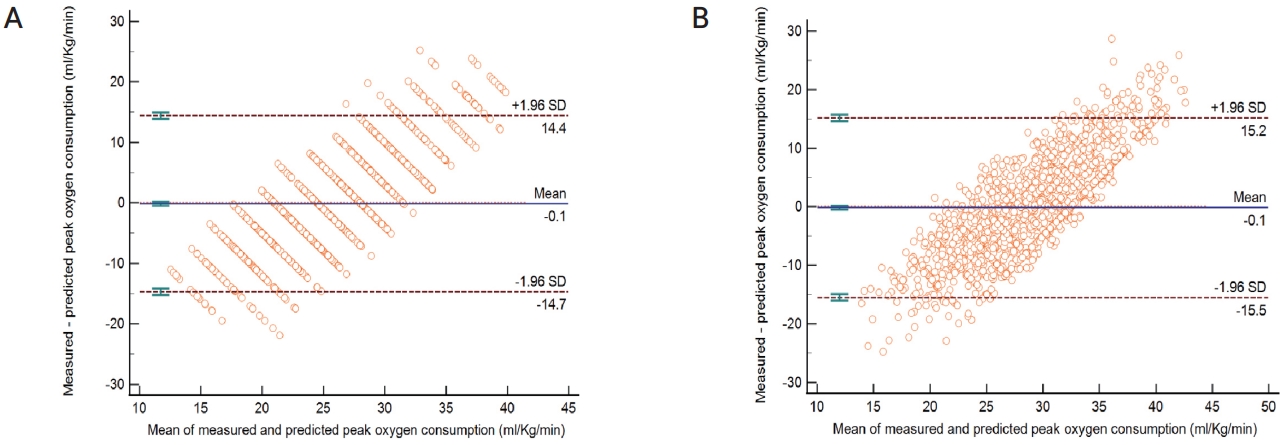
The Bland-Altman plots showing the level of agreement between the measured and predicted VO2peak values during the first and second visits are shown in Fig. 3. There was no significant mean difference between the predicted and measured VO2peak (on average, the predicted overestimated measured VO2peak_1 was 0.14 mL kg-1 min-1 , and the 95% CI was -0.17 to 0.45; P =0.37; VO2peak_2 was 0.15 mL kg-1 min-1 , and the 95% CI was -0.17 to 0.47; P =0.37), and the 95% limits of agreement of the differences between the two measurements were wide (14.4 to -14.7 mL kg-1 min-1 , 15.2 to -15.5 mL kg-1 min-1 ). The predicted-measured VO2peak was negatively correlated with the measured VO2peak. The predicted VO2peak tended to further underestimate the measured VO2peak as the measured VO2peak increased.
DISCUSSION
To the best of our knowledge, this study is the first to investigate the association between a self-reported activity status questionnaire (i.e., K ASI) and the CPET gold standard in patients after AMI. Our study demonstrated an association between the two tools for measuring functional status in patients with AMI. We found that both the KASI scores assessed at 1 and 3 months after AMI were significantly correlated with the measured VO2peak values. Based on these results, we revealed a linear relationship between these two measurements and derived an equation that predicts VO2peak using the KASI score for each period.
Several previous studies have examined the correlation between self-reported questionnaires that evaluate functional status and the CPET gold standard [15,21,22]. Li et al. [15] assessed whether the DASI, a patient-administered questionnaire, was accurate in predicting VO2peak objectively measured using CPET in 43 patients scheduled for elective major cancer surgery. According to this study, both the limits of agreement and bias between the measured and DASI-predicted VO2peak were large. They also showed that the DASI-predicted VO2peak generally tended to over predict the actual VO2peak values. Ravani et al. [22] also investigated the relationship between the VO2peak values predicted from the DASI questionnaire and those measured with CPET in 20 patients with stage 3-4 chronic kidney disease, and found that the DASI-estimated VO2peak tended to overestimate the measured VO2peak by approximately 4.3 mL kg-1 min-1 .
In contrast, our study showed that there was no significant difference in the mean bias for VO2peak between the two measurements; the mean bias in VO 2pea k was 0.1 mL kg-1 min-1 . Moreover, the correlations between the two measurement values obtained at different times showed similar results. These findings may have important implications for the clinical use of KASI.
We also revealed that the predicted VO2peak was negatively correlated with the measured VO2peak with wide limits of agreement. This pattern indicated underestimation at high VO2peak and overestimation at lower VO2peak values of the KASI-predicted VO2peak in patients with AMI. Potential causes of error contributing to the wide limits of agreement may have included the following. First, because of the nature of a multicenter study, several KASI interviewers were involved in this study. Since different interviewers collected the KASI data at each hospital, each of them may have explained the KASI item to the patient in a different way or may have underestimated or overestimated the patient’s response. Second, some participants found it difficult to answer the questionnaire because they did not accurately remember completing certain physical tasks specified in the questionnaire. Third, there could be significant discrepancies between the clinician’s assessment and self-report questionnaire when evaluating functional capacity [23,24]. Finally, this pattern may also be explained by the KASI, which was developed for patients with CVD, and not specifically for patients with myocardial infarction [16].
Nevertheless, the present results are significant in at least two major aspects. This is the first study to assess the relationship between KASI and CPET, which is particularly meaningful as CPET is often impractical because of the cost, time, expertise, and technological resources required. Additionally, the large-scale multicenter registry nature of our study, including a large number of hospitals across the country, offers greater generalizability among patients with AMI in Korea. In particular, it is possible to suggest that in patients with AMI with average-level functional capacity, the KASI scores tend to more closely reflect the relationship between the expected physical capacity and actual VO2peak.
However, the current study has several limitations. First, as mentioned earlier, owing to the multicenter nature of this study, interview bias may have been present. However, to solve this issue and maintain registry quality, we attempted to regularly educate all coordinators on the follow-up manual, error prevention, and data status. Second, the results of the current study are not representative of all patients with AMI. The generalizability of our findings to women with AMI participating in these assessments is limited, as 85% of our cohort were male. This finding is similar to that of previous studies that have suggested that the rates of CR enrollment among women are significantly lower than those of men [25,26]. Future studies examining sex differences in VO2peak values derived from the KASI in comparison to actual VO2peak using CPET are needed. Finally, most of the hospitals in the RCCs were tertiary centers with qualified critical pathways, supporting facilities, and specialized personnel. Therefore, caution should be exercised when the results of this study are applied to groups with different clinical characteristics.
As the importance of CR is emphasized in patients with AMI, the need for tools to assess functional status and HRQoL is increasing. For clinicians working with patients with reduced functional capacity, such as those with AMI, it is important to know the degree of actual functional ability of each patient. This study demonstrated that the KASI, a self-administered questionnaire, is a valid measure for the follow-up evaluation of the functional capacity of patients. These findings suggest that VO2peak can be predicted using the KASI in patients who do not undergo CPET. However, it should be noted in the KASI interpretation that the KASI score derived from VO2peak represents an average rather than individual-level change in VO2peak among patients with AMI.
This study aimed to determine the relationship between the KASI scores and CPET findings in patients with AMI, and we demonstrated that the KASI test could be a safe and cost-effective method for assessing functional capacity. The results of this study suggest that the KASI is a clinically reliable and useful evaluation tool compared to CPET, especially in patients with AMI. These results provide considerable convenience and clinical implications for the future. The KASI can also be a useful tool for clinical use and large-scale epidemiological studies.
Acknowledgements
This work was supported by a research grant from Jeju National University Hospital in 2019.