Vesicoureteral reflux-associated hydronephrosis in a dialysis patient treated with percutaneous nephrostomy
Article information
Abstract
Patients with vesicoureteral reflux (VUR), the retrograde flow of urine from the bladder to the kidney, are known to experience renal scarring; this results in the worsening of renal function. Reflux nephropathy is a cause of chronic kidney disease, and VUR has also been observed in dialysis patients. VUR is a major underlying precursor condition of urinary tract infection (UTI) and is sometimes accompanied by hydronephrosis. However, there are no guidelines for the management of UTI due to VUR-associated hydronephrosis in patients with end-stage kidney disease. Herein, we report a case of UTI caused by VUR-associated hydronephrosis in a dialysis patient treated with percutaneous nephrostomy.
INTRODUCTION
Vesicoureteral reflux (VUR) is a condition in which the retrograde flow of urine from the bladder into the ureter and toward the kidney, and it is known to be associated with urinary tract infection (UTI) [1]. Reflux nephropathy is renal scarring that is diagnosed in patients with VUR and accounts for 12-21% of chronic kidney disease in the pediatric population [2,3]. In general, the urine volume in dialysis patients without residual renal function is less than 100 mL per day [4]. Therefore, the incidence of UTI in end-stage renal disease (ESRD) is lower than that in the general population [5,6]. However, there are no optimal guidelines for the management of UTI in patients with VUR-associated hydronephrosis. Herein, we report a rare case of UTI in a patient with ESRD without residual renal function, which was treated with percutaneous nephrostomy (PCN) placement.
CASE REPORT
A 62-year-old Korean man undergoing hemodialysis visited the emergency department due to fever and left flank pain. His original disease was suspected to be VUR, which was diagnosed in his teenage years. He had undergone an anti-reflux operation for VUR 40 years ago and had received regular hemodialysis for 10 years. The patient maintained PCN for 2 years before and after dialysis initiation. During the period of maintaining PCN, the patient experienced UTI caused by methicillin-sensitive Staphylococcus aureus and was treated with the appropriate antibiotic therapy and removal of the PCN. Abdominal computed tomography (CT) performed 8 years ago did not reveal hydronephrosis.
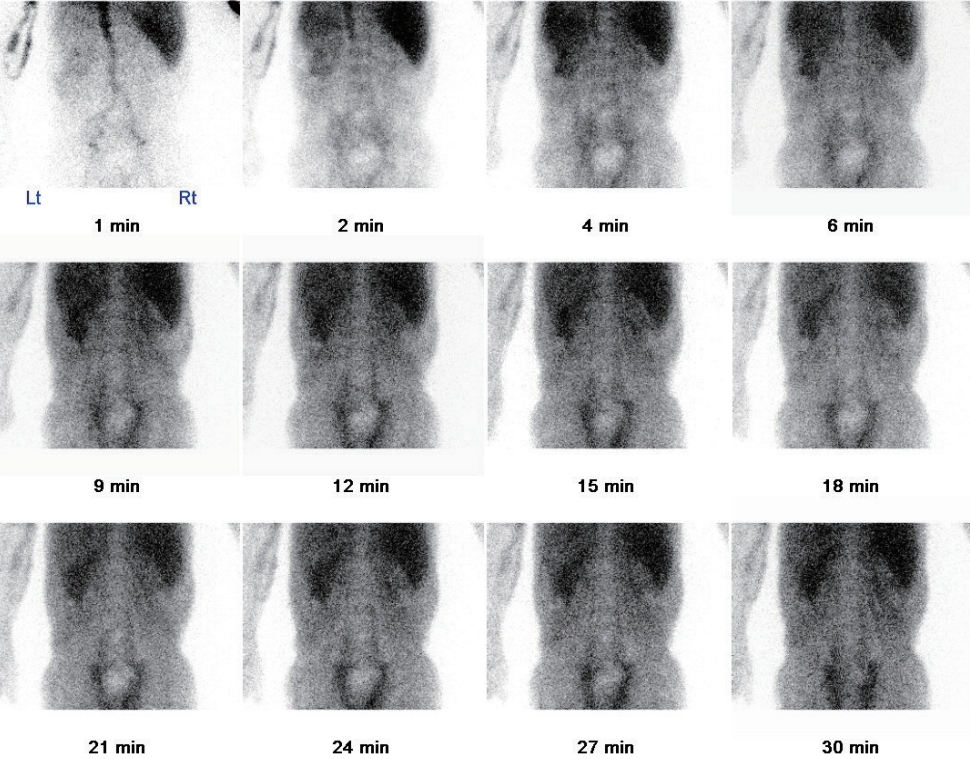
On admission, his initial vital signs indicated a blood pressure of 130/80 mmHg, heart rate of 80 beats per minute, temperature of 38.4°C, and respiratory rate of 20 breaths per minute. Physical examination revealed left costovertebral tenderness that was most apparent in the left f lank area. Laboratory testing revealed leukocytosis (white blood cell count: 13.1×103/mL), and the serum C-reactive protein level was 10.58 mg/dL (reference: <0.3 mg/dL). Urine sample was collected by clean catheterization and appeared pus- like, suggestive of UTI. Abdominal CT revealed a grade VVUR, hydronephrosis of the left kidney, and atrophy of the right kidney (Fig. 1A). Therefore, PCN was performed on the left kidney for UTI management due to hydronephrosis, and 2-g dose of intravenous ceftriaxone was administered concomitantly. Analysis of puslike fluid drained via PCN revealed a white blood cell count of 28.58×103 cells/µL, with 93% consisting of neutrophils. Urine culture was positive for Streptococcus dysgalactiae, which is sensitive to ceftriaxone, and bacterial growth was more than 106 CFU/mL. Although Tc-99m mercaptoacetyltriglycine renal scintigraphy revealed that both kidneys were in a near-nonfunctioning state, the volume of urine excreted through PCN did not exceed 80 mL/day during hospitalization (Fig. 2). Follow-up non-contrast-enhanced CT of the abdomen was performed on day 13 and revealed no dilatation of the bilateral renal pelvis and ureter (Fig. 1B). After the appropriate treatments including PCN and antibiotics, the patient showed subsequent improvement in symptoms and laboratory results and was discharged on day 14. Although we recommended removal of the PCN catheter, he insisted on maintaining this to prevent VUR-associated hydronephrosis. Thus, the patient was discharged with a PCN catheter and underwent PCN catheter exchange every 3 months. At the 12-month follow-up, the patient was doing well, without UTI recurrence. Ethical approval has been exempted by Institutional Review Board (IRB) of the Presbyterian Medical Center for reporting this case (IRB No. E2022-054).
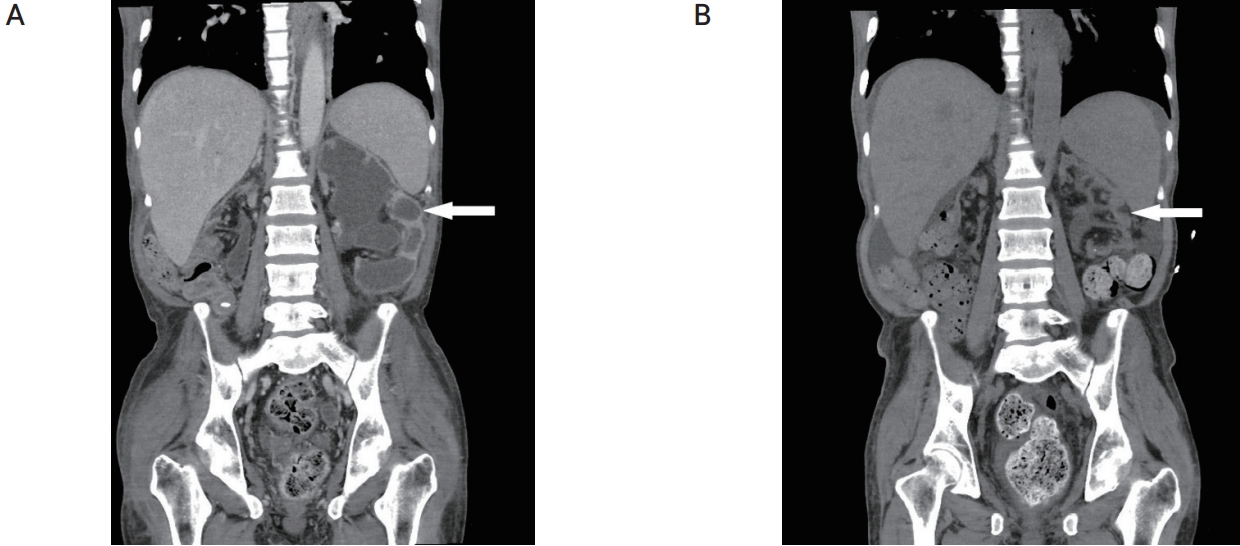
(A) Severe left hydronephrosis is shown in the abdominal computed tomography (CT) scan (arrow). (B) Follow-up CT scan reveals the disappearance of hydronephrosis after percutaneous nephrostomy insertion (arrow).
DISCUSSION
Primary VUR is the most common congenital urinary tract abnormality in childhood, and is commonly diagnosed after an episode of UTI, resulting in reflux nephropathy from renal scarring in association with UTI [1]. Approximately 5% of patients of all ages listed had chronic kidney disease due to reflux nephropathy, 7) and the incidence of VUR in ESRD patients has been reported to reach up to 30% [8]. However, there are no guidelines for the management of UTI due to VUR-associated hydronephrosis in patients with ESRD. We reported a case of VUR-associated hydronephrosis in a dialysis patient who was treated with PCN without residual renal function.
The incidence of UTI among hemodialysis patients has been reported to range from 22.5-33.0% [9]. The immunological profile of ESRD patients is compromised with regard to cell-mediated and humoral immunity. Apart from the reduced host immunity associated with chronic kidney disease, comorbidities including diabetes mellitus, urinary tract obstruction, and ref lux disease are risk factors for UTI [10]. Furthermore, a postvoiding residual urine volume greater than 50 mL is known to be a risk factor for the recurrence of UTI [9]. Recently, Yamashita et al. [9] reported that UTI can occur in hemodialysis patients with a small volume of urine, in which the daily urine output ranged from 20-1,300 mL. In addition, early diagnosis of UTI in hemodialysis patients may be easily neglected because the symptoms are usually subclinical [9]. Such findings were also observed in our case. Therefore, we believe that it is important to check for UTI even in dialysis patients with small urine output volumes.
Relief of urinary obstruction is the most common indication for PCN placement, representing 85-90% of patients [11], which was also the case in our patient. The patient in the present case had V UR-associated hydronephrosis despite not having residual renal function. We believe that the accumulation of a small amount of urine over several years may have contributed to hydronephrosis, as the PCN catheter was removed from the patient 8 years prior. Although the patient had to change his PCN catheter every 3 months, he was doing well without infection. Therefore, in special clinical circumstances, we believe that PCN may be an option for preventing repeated UTI in dialysis patients with VUR-associated hydronephrosis.
In summary, we report a rare case of UTI in a hemodialysis patient with VUR-associated hydronephrosis, in which UTI was successfully treated with the appropriate antibiotics and PCN.