Ultrasound-assisted subarachnoid block in a patient with severe kyphosis
Article information
Abstract
Here, we report a case of ultrasound-assisted subarachnoid block in a patient with severe kyphosis. A 69-year-old man was scheduled for metal removal from hip screws. He had a previous experience with subarachnoid block using the landmark-guided technique, but it was very difficult due to severe kyphosis. However, we could easily determine the correct needle insertion point using ultrasound imaging and performed a successful dural puncture on the first attempt. This case demonstrates the clinical usefulness of ultrasound imaging for subarachnoid blocks in patients with severe kyphosis.
INTRODUCTION
Subarachnoid block is a useful anesthetic method for lower abdominal and lower extremity surgery. It is traditionally performed using the landmark-guided technique, but may be unsuccessful and potentially unsafe in patients with severe kyphosis due to distorted spinal anatomy. Recently, ultrasound imaging has been gaining acceptability to facilitate subarachnoid block in patients with difficult spinal anatomy [1,2]. We report an interesting case of successful ultrasound-assisted subarachnoid block in a patient with severe kyphosis who had a previous experience of a difficult subarachnoid block using the conventional technique.
CASE REPORT
This case report was approved by the Institutional Review Board (IRB) of Jeju National University Hospital (IRB No. 2022-02-016) and the requirement for obtaining informed consent was waived.
A 69-year-old man, 124 cm in height and 28 kg in weight, was scheduled to undergo metal removal from hip screws. The patient had severe kyphosis (Fig. 1). A pulmonary function test revealed the presence of restrictive pulmonary disease, but the patient had few respiratory problems.

Photograph and radiographs of a patient with kyphosis. (A) Photograph of the patient. (B) Radiograph of thoracolumbar spine: lateral view. (C) Radiograph of the thoracolumbar spine: anteroposterior view.
Two years prior, he had undergone closed reduction internal fixation for a left femoral neck fracture. At that time, a subarachnoid block was perfor med using the landmark-guided technique, which proved very difficult. Several attempts of needle insertion at the suspected L3-4 and L4-5 interspaces with median and paramedian approaches were attempted for 30 minutes. Finally, a subarachnoid block could be achieved at the suspected L4-5 interspace with the median approach. The patient said that the previous experience had been tough, but he did not want general anesthesia for the current surgery. Considering his opinion and medical condition, we decided to attempt a subarachnoid block using ultrasound imaging.
When the patient entered the operating room, routine monitoring systems, including electrocardiography, pulse oximetry, and non-invasive blood pressure, were started. The patient was placed in a seated position. His lumbar spine was inwardly curved and flexion of the lumbar spine was not sustained. The midline, based on spinous processes, was identifiable, but the interspinous spaces for needle placement were poorly palpable.
Pre-procedural ultrasound images of the lumbar spine were obtained using a curved 2-5 MHz probe (SonoSite M-Turbo ®, SonoSite Bothell, WA, USA). The spinous processes were identified in the transverse spinous process view (Fig. 2A), and the neuraxial midline, composed of connecting spinous process tips, was marked. Then, the L4-5 interspinous space was determined using the sagittal spinous process view (Fig. 2B). The parasagittal oblique view showed that the L4-5 interlaminar space was appropriate for puncture, and the depth from the skin to the spinal canal was measured at 4 cm (Fig. 2C).
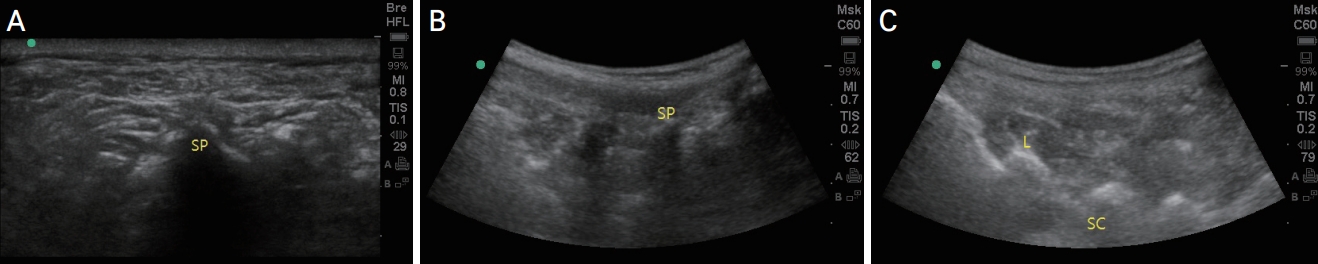
Ultrasound imaging of the lumbar spine. (A) Transverse spinous process view. (B) Sagittal spinous process view. (C) Parasagittal oblique view. SP: spinous process, L: lamina, SC: spinal canal.
After determining the needle insertion point, a 25-gauge Quincke spinal needle was introduced via the median approach to the L4-5 interspinous space. At a depth of approximately 4 cm, the backflow of cerebrospinal fluid was obtained in the first attempt. He was placed in the left lateral position after injecting 8 mg of 0.5% hyperbaric bupivacaine. A subarachnoid block was successfully achieved at the dermatome level of T6. The surgery proceeded uneventfully, and the patient recovered from the block without complications.
DISCUSSION
In the present case, the midline based on the spinous processes was identifiable, but the interspinous spaces for needle placement were poorly palpable. Ultrasound aided in the identification of interspinous spaces, and the spinal needle could be easily introduced into the midline and we successfully performed a dural puncture on the first attempt.
Subarachnoid block is a useful anesthetic method for lower abdominal and lower extremity surgery. It could be a superior option for patients with severe kyphosis, who are more likely to suffer from respiratory complications after general anesthesia. The subarachnoid block is traditionally performed using a land mark-guided technique. It is simple, fast, and effective in most patients. However, this conventional technique may be unsuccessful and potentially unsafe in patients with kyphosis due to distorted spinal anatomy. In these cases, fluoroscopy can be used to identify the small accessibility window, thereby facilitating the subarachnoid block; however, radiation exposure to patients and staff remains a concern [3,4].
Recently, ultrasound imaging has been more frequently used to improve the efficacy of subarachnoid block [1,5]. Ultrasound imaging can provide important clinical information, such as identification of intervertebral levels, determination of the needle insertion point, angle of needle trajectory, and depth of needle insertion. This can facilitate the subarachnoid block, particularly in patients with difficult surface anatomic landmarks [6,7].
Current data suggest that the use of ultrasound could reduce the technical difficulties associated with subarachnoid block in patients with difficult spinal anatomy, such as those with pregnancy, obesity, history of spinal surgery, and kyphoscoliosis. Creaney et al. [8] compared pregnant women with impalpable spinous processes undergoing caesarean delivery under spinal anesthesia and found that there were significantly fewer needle passes in the ultrasound group compared to the landmark palpation group. Li et al. [9] documented that ultrasound examination facilitated subarachnoid block in obese patients by improving the first-attempt success rate and reducing the number of needle passes. Another recent study conducted in patients with scoliosis or history of spinal surgery showed that the number of needle passes and puncture attempts were lower in the ultrasound group than in the conventional group [2].
Our report is unique in that we could easily determine the correct needle insertion point using ultrasound imaging, even though the previous subarachnoid block using the landmark-guided technique was very difficult to perform. This demonstrates the clinical usefulness of ultrasound-assisted subarachnoid block in patients with kyphosis.
In conclusion, a subarachnoid block in patients with kyphosis presents significant challenges for anesthesiologists. Ultrasound imaging should be routinely considered to improve technical performance in patients with similar spinal deformities.
Acknowledgements
This work was supported by the 2022 education, research and student guidance grant funded by Jeju National University.