Fertility-preservation laparoscopic management of an intact broad ligament abdominal ectopic pregnancy: a case report
Article information
Abstract
This study reports a rare case of broad ligament abdominal ectopic pregnancy (EP). Interventions included preoperative transabdominal and transvaginal ultrasonography and operative laparoscopy. Successful extraction of the EP, followed by suturing of the mesosalpinx, was performed. Laparoscopic fertility-preservation treatment of broad ligament EP is valuable for women during the childbearing period.
INTRODUCTION
Abdominal ectopic pregnancy (EP) represents only 1% of all EP cases. Broad ligament ectopic pregnancy is a rare subtype of abdominal EP, accounting for only 1% of all abdominal EP cases [1]. Despite its paucity, the maternal mortality rate has been reported to be as high as 20%, mostly because of misdiagnosis and spontaneous rupture [2]. However, studies on this topic are limited. Some authors have reported failed laparoscopic management and switch to laparotomy [3], while others have reported a successful laparoscopic approach, followed by successful subsequent intrauterine pregnancy [4]. Herein, we present a rare case of a patient with broad ligament EP who was seeking future fertility and was treated conservatively using a minimally invasive laparoscopic approach.
CASE REPORT
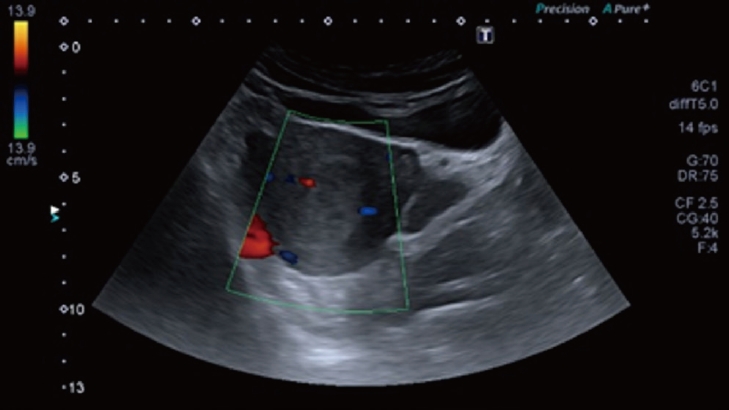
A 33-year-old woman, gravida 2 para 1, presented to the clinic with a positive urine pregnancy test result and a calculated gestational age of 6 weeks based on a reliable last menstrual period. She previously delivered vaginally 7 years ago, with an unremarkable medical, surgical, and family history. On transabdominal ultrasonography, no intrauterine gestational sac was noted, but definite decidua (thickened echogenic endometrium) (Fig. 1) was observed. No adnexal mass or fluid was identified in the pouch of Douglas. Clinically, the patient was calm and had no pain, lower abdominal tenderness, or other complaints. A serum β-human chorionic gonadotropin (β-HCG) test was requested, and the results was reported on the next day at 471.8 IU/L. She was recommended to undergo transvaginal ultrasonographic examination, which revealed no intrauterine gestational sac. However, a welldefined left adnexal mass, 2.8×2.5×1.2 cm, with an irregular echogenic border was noted, which was suggestive of chorionic tissue with a small non-pulsating fetal pole, as revealed by Doppler study (Fig. 2). Surprisingly, no left adnexal tenderness or free fluid was observed within the pelvic cul-de-sac. She was counseled for methotrexate versus laparoscopic intervention. She chose laparoscopy to search for any pathology causing secondary infertility, which she had experienced for 7 years despite repeated trials of ovulation induction with normal hormonal profile, semen analysis, and hysterosalpingography (HSG) findings. She was scheduled for a postmenstrual diagnostic and operative laparoscopy. After receiving insurance approval and anesthesia consultation, routine preoperative laboratory tests were performed, and the results were within normal limits. Diagnostic laparoscopy revealed dense left-sided omental adhesions masking the left adnexa and fine right-sided adhesions on the right adnexa and pouch of Douglas. These findings explained the prolonged period of secondary infertility. Adhesiolysis was performed using fine sharp dissection, followed by exploration of the left adnexa. The left fallopian tube appeared normal in caliber and patent upon saline injection via a cervical cannula. However, a vascular, 2 cm, left broad ligament mass was noted, with a definite bulge seen via both the anterior (Fig. 3A) and posterior (Fig. 3B) leaves of the upper part of the broad ligament (mesosalpinx). However, the largest lower portion of the broad ligament (mesometrium) was free. The ureter was examined and found to be away from the mesosalpinx. The uterus was enlarged and soft due to pregnancy. The procedure started by injection of copious amounts of a solution comprising 1 mL adrenaline, 25 mL xylocaine, and 50 mL saline 0.9% into the mesosalpinx, after indication from the anesthesia team to monitor the patient’s vital signs. Thereafter, the anterior leaf was opened with scissors (Fig. 4A), followed by extraction of the ectopic tissues with grasping forceps (Fig. 4B). After ensuring complete extraction of the tissues, meticulous hemostasis of the bleeding points was achieved using monopolar Maryland forceps. The edges of the peritoneum and the underlying connective tissue were sutured using a continuous 3/0 Vicryl stitch. The procedure ended with repeated suction irrigation and insertion of a soft suction drain. The estimated blood loss was 60 mL.
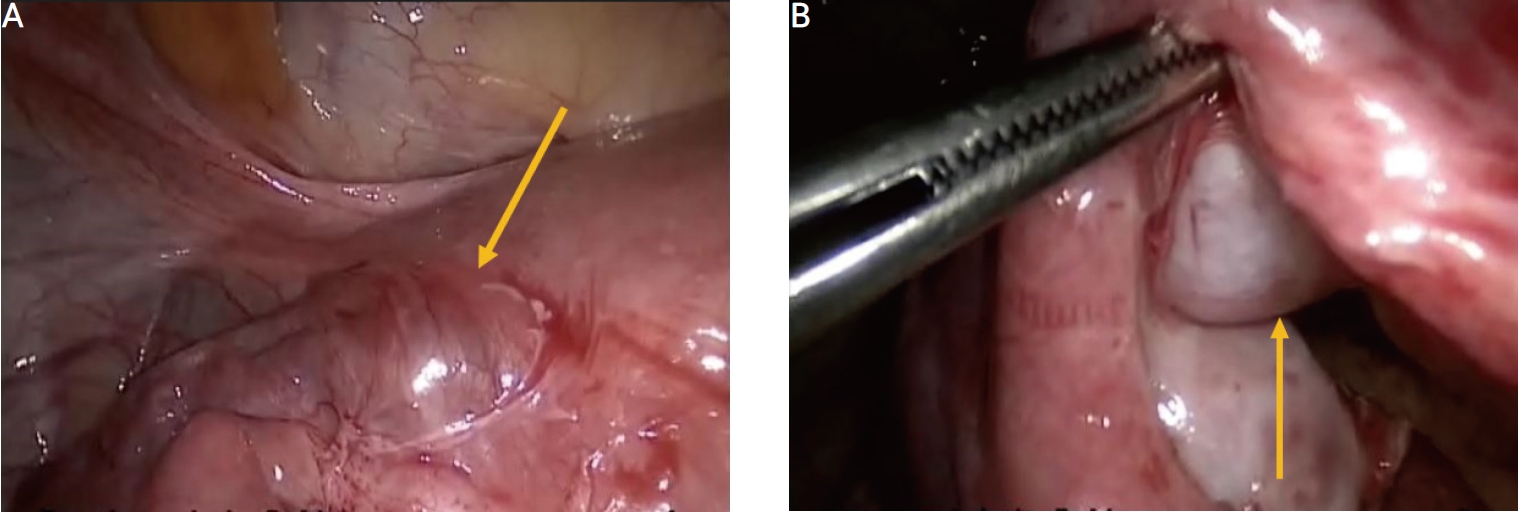
Laparoscopic appearance of left broad ligament ectopic pregnancy seen via anterior and posterior leaves (A and B, respectively).
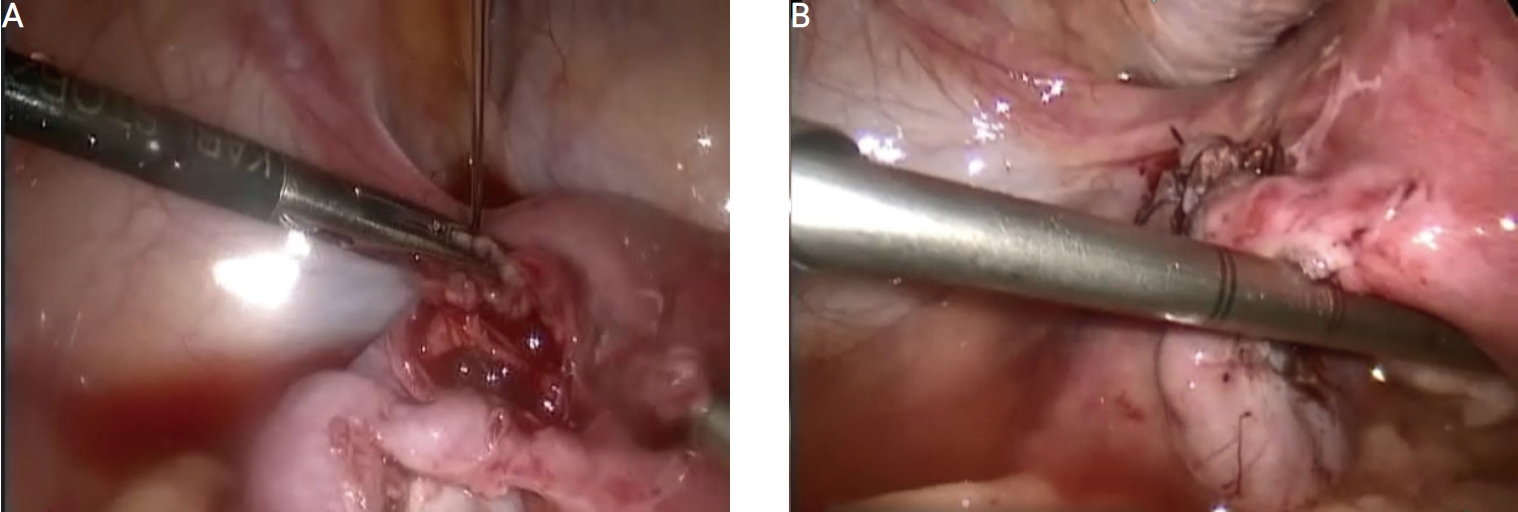
Steps of surgical extraction of ectopic pregnancy using a grasping forceps (A) and closure of the defect (B).
The patient tolerated the procedure well and was discharged on postoperative day 1. The final pathology showed remnants of the conception. The patient menstruated for 5 days, starting on postoperative day 2. Her serum β-HCG level returned to non-pregnant levels over the following month, and she was doing well at her 8-week follow-up visit. The patient provided written informed consent to publish this case report.
DISCUSSION
Rare sites of EP include interstitial, cervical, cesarean scar, cornual, ovarian, abdominal, and heterotopic pregnancies. Studies addressing broad ligament abdominal EP are expected to be scarce, with only case reports or small series [5]. The rarity of this type of EP makes it impossible to conduct prospective trials to determine the best possible treatment modality [6]. The exact mechanism underlying the occurrence of a broad ligament EP is uncertain. This may occur secondary to the downward rupture of tubal EP. Contrary to this theory is the occurrence of EP in a patient with a history of prior ipsilateral salpingooorectomy [1], which has been reported in a patient with a history of tubal sterilization [6]. In our case report, the fallopian tube was normal and intact, but we reported bilateral tubo-ovarian omental adhesions that would hinder normal fertilization at the tubal ampulla and help implantation into an abnormal site. Pelvic endometriosis has been poorly implicated in its causation [7]. In this case report, the preoperative β-HCG titer was low, requiring only follow-up or a single dose of methotrexate after exclusion of early intact intrauterine pregnancy or abortion. The first option was refused by the patient, as she was already worried about her fertility. Methotrexate therapy has been shown to be very effective in treating patients with a low β-HCG titer, those with a small mass size, and hemodynamically stable patients, as in the present case. However, in a previous randomized study, methotrexate was shown to be less effective than laparoscopy in treating EP [8]. A decision of laparoscopy as a first-line management at the patient’s request was helpful, as we detected bilateral adnexal and adhesions in the pouch of Douglas, explaining the prolonged infertility for 7 years, despite all attempts to have a natural pregnancy, with normal hysterosalpingography (HSG). These findings may explain the occurrence of EP. Concomitant adhesiolysis is considered as a preventive treatment method to avoid repeated EP. We believe that administering one or more doses of methotrexate would have masked the exploration of the cause of prolonged secondary infertility and detection of the possible etiology of EP. Moreover, persistence of pelvic adhesions is a definite risk factor for recurrent EP [9]. Additionally, early laparoscopic intervention may have prevented possible rupture and internal hemorrhage caused by the thin wall of the broad ligament, as reported previously [2,3]. In our present case, the small mass size supports this concept to avoid advanced and late intervention. Some case reports described aggressive surgery to manage this condition, such as removal of the broad ligament EP, partial cornual resection of the uterine serosa, oophorectomy, and bilateral salpingectomy as the vascular implants were extended in the infundibulopelvic ligament [3]. Others have described left adnexectomy after transperitoneal identification of the left ureteral path and removal of left broad ligament pregnancy with removal of the ectopic placenta [10]. The novelty of this case report is the description of a conservative fertility-preserving technique initiated by injection of copious amounts of hemostatic agents to minimize bleeding, the use of fine scissors to open the anterior leaf of the broad ligament, and the ensured farness of the ureter. Additionally, the meticulous closure of the defect in a microsurgical manner avoided adhesion formation and, most importantly, kept the ipsilateral fallopian tube in a good condition. Furthermore, this case report highlights the importance of available expert laparoscopists in some cases of EP for adhesiolysis and in dealing with abnormal localization of the ectopic sac.
Acknowledgements
The author thanks the patient for agreement to publish her case.