Isolated distal vaginal hypoplasia and megalourethra in a regularly menstruating female treated by pull through procedure
Article information
Abstract
This case report describes a case of isolated (not associated with other anomalies) lower vaginal hypoplasia complicated by megalourethra (urethral dilatation) due to frequent urethral sexual intercourse in a regularly menstruating (hypomenorrheic) woman. The patient was a 24-year-old woman who underwent transperineal ultrasonography as well as magnetic resonance imaging followed by sequential cystoscopic and vaginoscopic examinations. Finally, a pull-through procedure was used to create a new vagina. The main outcome measure was patent vagina formation. The procedure successfully corrected isolated lower vaginal hypoplasia. The postoperative course was smooth, with the restoration of regular intercourse in the correct location. It was concluded that all gynecologists should have increased awareness of rare female genital anomalies to avoid serious sequelae, particularly in newly married patients.
INTRODUCTION
Isolated congenital lower vaginal atresia is a rare congenital defect due to failure of canalization of the urogenital sinus, resulting in vaginal outf low tract obstruction. Clinically, it presents with primary amenorrhea, cryptomenorrhea, apareunia, and cyclic chronic pelvic pain [1]. Lower vaginal hypoplasia is a rare subtype of congenital lower vaginal atresia. There is no single publication in the English literature on isolated congenital vaginal hypoplasia. Moreover, neither the female genital tract anomalies nor the urogynecologic anomaly classifications address lower vaginal hypoplasia [2].
CASE REPORT
A 24-year-old patient complained of primary infertility for 6 years despite continuous marital life. The male factor was excluded by normal semen analysis twice. Upon vaginal examination, an incomplete imperforate hymen was excluded by visualization of a torn hymenal ring at the site of the vaginal opening. There was no vagina; however, there was an anterior dilated oblong opening just below the clitoris up to one finger breadth, which could be dilated up to two fingers. The patient was again asked about her menstrual history; however, she confirmed that she was regularly menstruating. Upon repeated inquiry, she mentioned that the menstrual flow slowly comes only during micturition, but from the vagina, and that the amount of menstruation was minimal (hypomenorrhea). The patient reported no hematuria. Regarding sexual history, she experienced apareunia at the beginning of her marital life, which slowly improved over time. Thereafter, she reported marked dyspareunia, followed by incontinence with a large amount of urine during intercourse. Both partners were satisfied only when the patient’s urinary bladder was empty. She reported occasional external (clitoral) orgasms, despite superficial dyspareunia. Clinically, the patient showed no evidence of virilization. Transperineal ultrasonography and magnetic resonance as magnetic resonance imaging revealed a normal-sized uterus and ovaries in addition to a normal upper vaginal cavity without dilatation or hemorrhage in the uterine cavity, cervical canal, or upper vaginal segment. Transabdominal ultrasonography excluded the associated renal anomalies.
The patient underwent vaginal exploration under general anesthesia after obtaining written consent. Under spinal anesthesia, after proper sterilization, the central orifice was presumed to be the vagina (Fig. 1A). It accepted one finger easily and could be dilated into two fingers. Utilizing a 2.6 mm telescope and a 3.2 mm diagnostic sheath, endoscopic evaluation revealed a bladder wall with definite ureteric orifices Figure 1B as a proof that it was a dilated urethra (megalourethra). After leaving the bladder, the telescope was moved backwards, followed by trials searching for vaginal orifices that succeeded in finding a lateral leftsided dimple just behind the large urethral orifice (Fig. 1D). It was inflated with saline irrigation followed by proper visualization of the fornices and cervix (Fig. 1C) using the mini-vaginoscope technique as described by our team [3]. To avoid urethral or bladder injury, surgical correction was initiated by insertion of a urethral Foley catheter. Rectal injury was avoided by frequent insertion of a finger into the rectum to guide posterior dissection. Using alternating sharp and blunt dissection, the small dimple was dilated by dissecting the fibrous tissue, forming a reasonable canal. The latter was further dissected until it reached the upper vagina, forming a single tube. To avoid reformation of the stenosis, the normal upper vagina was connected to the new vaginal orifice using a pull-through technique as previously described [4]. At the end of the operation, a vaginal pack was inserted into the new vagina and removed upon discharge. The patient was kept on local povidone-iodine 10% vaginal douches, non-steroidal anti-inflammatory drugs and broadspectrum systemic antibiotics. The postoperative course of the patient was uneventful. 1 week later, the patient was examined and a normal vaginal caliber was confirmed. Notably, the urethral opening was nearly normal. On the tenth postoperative day, the couple was instructed to practice proper intercourse. 2 months later, the patient became pregnant, and a cesarean section was performed at the end of the 39th week for mild pre-eclampsia.
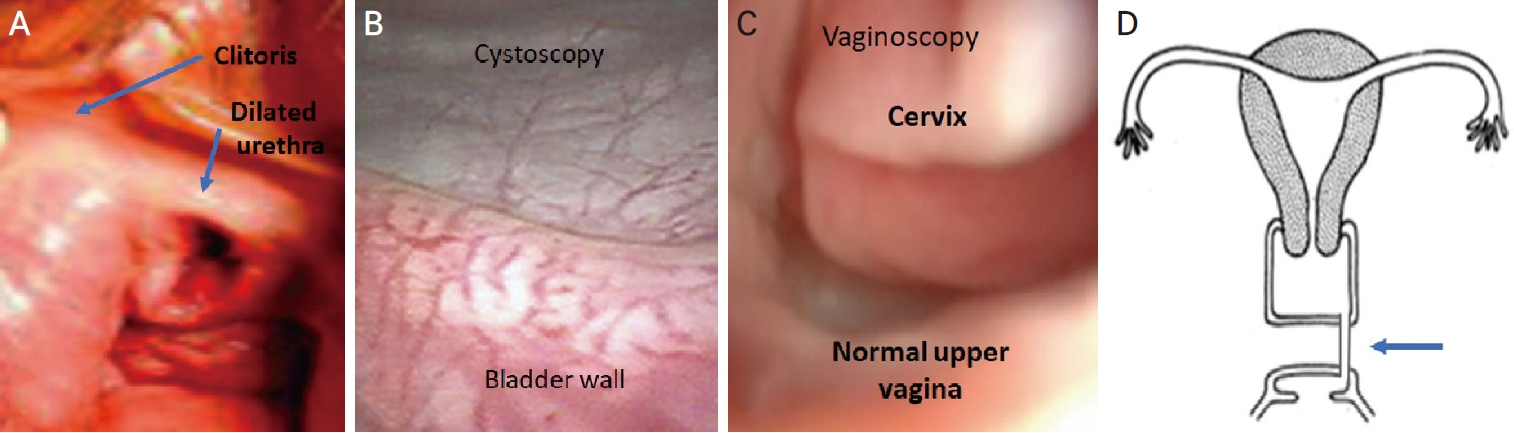
(A) The gross appearance of the dilated urethral opening. (B) Endoscopic image through the urethral opening revealed a bladder with well seen ureteric orifices. (C) Vaginoscopic appearance of normal upper vagina, fornices, and the cervix. (D) A diagrammatic view of the left lateral tubular canal connecting to the upper vagina (arrowed).
DISCUSSION
A normal vaginal is formed after fusion of the lower part which is developed from the urogenital sinus and upper part which is developed from the Müllerian duct followed by recanalization and resorption of the meeting membrane. Vaginal aplasia or hypoplasia is a rare congenital anomaly of the lower vagina due to urogenital sinus non-development or poor development. Non-Müllerian malformations are not very common, but they do occur and are often incorrectly identified, inappropriately treated and sometimes incorrectly reported.5 Many classifications addressing female genital congenital anomalies have been published [5]. The most famous is the American Society of Reproductive Medicine (ASRM) classification but it poorly describes vaginal anomalies as a part of Müllerian duct agenesis [2]. Previously, we recommended addition of description of some rare anomalies like complete vaginocervicouterine septum to the old AFS classification [6]. The recent ASRM Müllerian anomalies classification in 2021 [2] added a subtype of this anomaly but didn’t add any section on vaginal aplasia. Even publications that criticized this classification [7] failed to address its lack of including varieties of lower vaginal anomalies. This can be attributed to the unique origin of the lower vagina from the urogenital sinus. However, the ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies described vaginal anomalies more broadly and considered V4 as an indicator of vaginal aplasia [8], but did not address vaginal hypoplasia. Our case report and others tried to direct attention of gynecologists to varieties of the urogenital sinus anomalies to be put in mind while evaluation any case of suspected genital tract anomalies. Some authors described congenital urogenital anomalies causing hemato/hydrocolpos mainly of four types; imperforate hymen, distal vaginal agenesis, transverse vaginal septum, and obstructed hemivagina and ipsilateral renal anomaly [9] without any comment on distal vaginal hypoplasia. Likewise, urogenital anomalies classifications ignore discussing vaginal atresia or hypoplasia [10] and focus on the relationship of true vaginal location according to the distance from the bladder neck to the vagina and the distance from the vagina to the perineal meatus, the external genital appearance and phallic length and width.
What’s new in this case is the description of distal vaginal hypoplasia rather than aplasia. To the best of our knowledge, this is the first case report of advanced distal vaginal hypoplasia in a regularly menstruating female associated with megalourethra due to wrong way of sexual intercourse for 5 years. This case report highlights the central medical position of gynecologists in the lives of many women as previously described [11]. In many hospitals, premarital counselling relies only on lab results. This case report raised an important issue of adding meticulous premarital clinical and transperineal and abdominal sonographic assessment is mandatory to rule-out any genital tract anomalies. Sex education regarding the best and safe approaches of intercourse, orgasm and other natural sexual functions should be included in all premarital programs. Lack of sex education and the misconception of the concept of sex education may lead to various negative problems [12,13]. Regardless fertility or contraception purpose, this case report demonstrated that early medical consultation for the newly married couples is highly recommended for early intervention at an appropriate time before occurrence of some complications like megalourethra which may develop due to wrong urethral intercourse. Due to anatomic and embryologic proximity, association of urinary tract problems with distal vaginal aplasia or hypoplasia raises the importance of urogynecologic assessment of any female with urinary symptoms as recorded in some case report [14].
Despite being very rare in females, megalourethra on sexual intercourse was previously reported in cases of vaginal agenesis [15,16], imperforate hymen, cribriform hymen, annular fibrotic hymen or microperforate hymen [17-19]. Hymenal abnormalities were excluded in this study by clinical visualization of hymenal remnants at the beginning of the vagina. Lower vaginal aplasia was excluded due to regular menstruation. Nevertheless, not all anomalies are identical as this case represents a very rare subtype of vaginal hypoplasia. The current case report describes megalourethra in a regularly hypomenorrheic female with advanced lower vaginal hypoplasia. Distal vaginal hypoplasia should be included in classifications of female genital anomalies to increase doctor awareness for early and proper management.